NYC's Top Crohn's Disease Specialists
Our board-certified, highly rated gastroenterologists have undergone rigorous training in the evaluation and treatment of a wide array of digestive diseases and are experts in inflammatory bowel diseases such as Crohn's disease and Ulcerative Colitis. Our goal is to provide safe and effective therapies in a warm and friendly environment.
 ★★★★★
Dr. Divya Mallam
Gastroenterologist
★★★★★
Dr. Divya Mallam
Gastroenterologist
 ★★★★★
Dr. Dana Zhao, MD
Gastroenterologist
★★★★★
Dr. Dana Zhao, MD
Gastroenterologist
 ★★★★★
Dr. Michael Rosman, MD
Gastroenterologist
★★★★★
Dr. Michael Rosman, MD
Gastroenterologist
 ★★★★★
Dr. Michael Schopis, MD
Gastroenterologist
★★★★★
Dr. Michael Schopis, MD
Gastroenterologist
 ★★★★★
Dr. Connie Park, MD
Gastroenterologist
★★★★★
Dr. Connie Park, MD
Gastroenterologist
 ★★★★★
Dr. Qin Rao, MD
Gastroenterologist
★★★★★
Dr. Qin Rao, MD
Gastroenterologist
 ★★★★★
Dr. Daniel Perl, MD
Gastroenterologist
★★★★★
Dr. Daniel Perl, MD
Gastroenterologist
 ★★★★★
Lauren Schwartz, MD
Gastroenterologist
★★★★★
Lauren Schwartz, MD
Gastroenterologist
 ★★★★★Eric Yoon, MD
Gastroenterologist
★★★★★Eric Yoon, MD
Gastroenterologist
 ★★★★★
Kristen Lee, MD
Gastroenterologist
★★★★★
Kristen Lee, MD
Gastroenterologist
 ★★★★★
Mikhail Yakubov, MD
Gastroenterologist
★★★★★
Mikhail Yakubov, MD
Gastroenterologist
 ★★★★★
Michael Dann, MD
Gastroenterologist
★★★★★
Michael Dann, MD
Gastroenterologist
 ★★★★★
Shawn Khodadadian, MD
Gastroenterologist
★★★★★
Shawn Khodadadian, MD
Gastroenterologist
 ★★★★★
Aga Nagorna, MD
Gastroenterologist
★★★★★
Aga Nagorna, MD
Gastroenterologist
 ★★★★★
Kathryn Schmidt, MD
Gastroenterologist
★★★★★
Kathryn Schmidt, MD
Gastroenterologist
What is Crohn’s Disease?
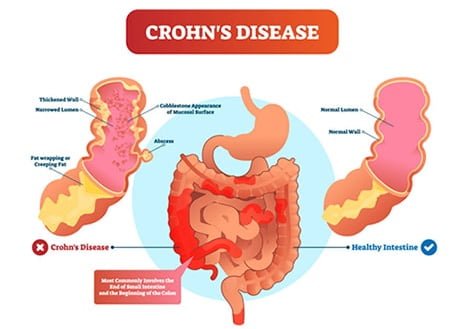
Crohn’s disease is an inflammatory bowel disease (IBD) that often affects the lining of your large or small intestine. When it strikes, it spreads deep into the tissue, causing ulcerations and damage. This medical condition impedes your body’s ability to digest food, resulting in abdominal pain, severe diarrhea, rectal bleeding, and malnutrition. Suppose you have symptoms that could be consistent with Crohn’s disease or have already been diagnosed. f you have Crohn’s disease-like symptoms or have previously been diagnosed with it, you should always be evaluated by a physician for an accurate diagnosis and treatment plan, as well as to rule out a more serious or urgent condition.
Crohn’s disease can affect any part of your digestive tract, from your mouth to your anus.
”
★ ★ ★ ★ ★The entire staff was welcoming and made the visit quick and seamless. The office is clean, and the staff even make a point in offering coffee or water while you wait. The doctor was very friendly and to the point. Highly recommend choosing this office.
How Common Is Crohn’s Disease?
Crohn’s disease is quite common. Approximately 2.5 million U.S. citizens were diagnosed with IBD (either ulcerative colitis or Crohn’s disease) in 2020. Experts estimate that the number of people living with IBD in the United States will reach 3.5 million by 2030.
Crohn’s Disease Symptoms
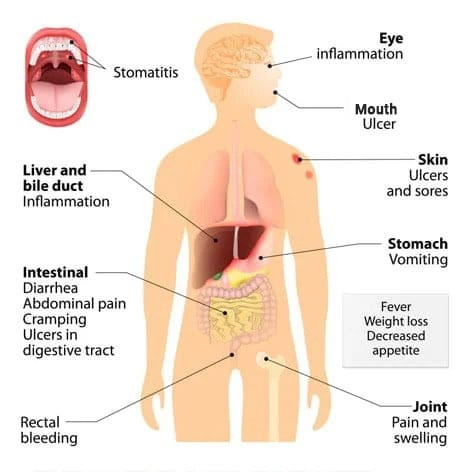 Crohn’s disease affects different intestinal spots in different people. Common symptoms include:
Crohn’s disease affects different intestinal spots in different people. Common symptoms include:
- Abdominal pain;
- Blood in your stool;
- Cramping;
- Loss of appetite;
- Ulcers, even in your mouth;
- Unexplained weight loss;
- Diarrhea, sometimes repeatedly.
Less common symptoms include blocked bowels, fever, fatigue, skin problems, inflamed liver, and arthritis. Cigarette smoking, infections, or hormonal fluctuations can all aggravate Crohn’s disease.
Causes of Crohn’s Disease
Although the exact cause of Crohn’s disease is unknown, stress and diet are not the culprits, as previously believed. The two most likely causes are an improperly functioning immune system or heredity. Both of these are still theories at this point.
You are more likely to get Crohn’s disease if you fall into one of these categories:
- Not yet 30 years old
- Descended from Eastern European (Ashkenazi) Jews
- A family member has it
- Cigarette smoker
- Live in a northern climate
- Live in a city or urban area
What to Expect at Your First Visit
The initial assessment for Crohn’s disease would involve discussing your symptoms and any treatments you’ve tried and taking your medical history. Share detailed information about the type, location, duration, and intensity of your symptoms. Your specialist may also ask about your family history of digestive diseases or related issues.
Next, a physical examination will take place. This would involve inspecting and palpating your abdomen to check for any tenderness, pain, lumps, or other abnormalities. Your doctor may also check your vital signs, including blood pressure and heart rate before proceeding with diagnostic tests.
Diagnosing Crohn’s Disease
Besides physical exams, our NYC Crohn’s disease specialists use several other methods to diagnose your problem, as it may resemble other conditions. Some other tests include:
- Colonoscopy
- Endoscopy
- Enteroscopy
- Biopsy tissue sample
- Blood tests
- Small bowel capsule
- Stool sample analysis
- Imaging
Broadly speaking, Crohn’s Disease can be characterized as the following:
- Inflammatory Crohn’s Disease characterized by diarrhea that is sometimes bloody;
- Structuring Crohn’s disease characterized by scarring and fibrosis of the intestine, resulting in blockage and crampy abdominal pain;
- Fistulizing Crohn’s abnormal channels or tracts that form between adjacent bowel loops or between the bowel and the skin. Often, the three types co-exist to some extent.
Discover the article: Common Crohn’s Disease Food Triggers
Treating Crohn’s Disease
There is no known cure for Crohn’s disease. Drugs can sometimes result in long-term disease remission, helping control your symptoms and limiting complications. Many patients with Crohn’s disease are able to return to their everyday lives.
Medications for Crohn’s Disease:
Medications for Crohn’s disease work by targeting different aspects of the inflammatory process. They include:
- Anti-inflammatory Drugs:
These are often the first line of treatment for mild to moderate Crohn’s disease.
Aminosalicylates, such as sulfasalazine and mesalamine, help reduce inflammation in the lining of the intestines. - Biologics:
Biologics are a class of medications that target specific proteins involved in the inflammatory process. Biologics are typically used for moderate to severe Crohn’s disease or when other medications have failed.
They include TNF inhibitors (e.g., infliximab, adalimumab), anti-integrins (e.g., vedolizumab), and anti-interleukin-12/23 antibodies (e.g., ustekinumab). - Steroids and Immunosuppressants:
Corticosteroids, such as prednisone, are potent anti-inflammatory drugs used to induce remission during flare-ups. However, they are not intended for long-term use due to potential side effects.
Immunosuppressants, such as azathioprine and methotrexate, suppress the immune system to reduce inflammation. They are often used in combination with biologics or to maintain remission.
If medical therapy fails, surgery may be an option if the damage to your intestines is localized. We can surgically remove the affected area, but this does not guarantee that the disease will not recur in another part of your intestines.
When Surgery is Necessary:
- Complications such as strictures (narrowing of the intestines), fistulas (abnormal connections between organs), abscesses (collections of pus), and intestinal obstructions may require surgical intervention.
- Failure of medical therapy.
- Severe bleeding.
Types of Surgical Procedures:
- Strictureplasty: Widens narrowed sections of the intestine.
- Resection: Removes diseased portions of the intestine.
- Fistulotomy: Repairs fistulas.
- Colectomy: Removal of the colon.
- Ileostomy or Colostomy: Diverts stool through an opening in the abdomen.
Finally, because Crohn’s disease increases the risk of colorectal cancer, you should get more frequent colon cancer screenings. You should discuss your screening regimen with your gastroenterologist.
Types of Crohn’s Disease
There are five types of Crohn’s disease, each affecting different digestive tract sections and causing unique symptoms.
- Ileocolitis is the most common type that affects the last and the longest part of the small intestine (ileum) and the beginning of the large bowel. The symptoms of Ileocolitis include weight loss, cramping, diarrhea, and pain in the lower right side of the abdomen.
- Ileitis affects only the small intestine. It typically leads to the same symptoms as Ileocolitis, but you may also develop abdominal fistulas or abscesses.
- Crohn’s Colitis occurs due to inflammation in the main part of the large intestine and is characterized by the formation of abscesses, fistulas, and ulcers around the anus as well as skin sores, rectal bleeding, and joint pain.
- Jejunoileitis typically affects the middle part of the small intestine (jejunum) and results in abdominal cramps and pain after meals as well as diarrhea and formation of fistulas.
- Gastroduodenal Crohn’s Disease is a rare type that affects the duodenum, the small intestine’s first C-shaped segment. Key symptoms include abdominal pain, nausea, vomiting, decreased appetite, and associated weight loss.
Different types of Crohn’s Disease are prevalent in patients of different ages, and some may develop due to other conditions. Visit Manhattan Gastroenterology for a comprehensive health check-up to ensure proper diagnosis and avoid severe complications.
Common Complications of Crohn’s Disease
Although Chron’s disease is not a terminal illness, it can lead to serious or even fatal consequences, such as:
- Bowel obstructions – narrowed areas within the intestinal passage that arise from swelling and development of scar tissue, making it difficult for food to pass through. In severe cases, they may cause a complete blockage.
- Fistulas – tracts connecting different intestine parts that develop from sores or ulcers and often become infected.
- Anal fissures – cracks or tears developing exclusively in the area of the anus.
- Abscesses – pus-filled pockets of infection localized in the intestinal wall.
- Malabsorption and malnutrition – conditions that cause inadequate dietary intake, intestinal loss of protein, and poor absorption of nutrients.
- Bile salt malabsorption – a disease in which acids are not properly reabsorbed from the ileum and instead flow into the large intestine, causing stomach problems and diarrhea.
If you start to experience any of the above-mentioned symptoms, it is critical that you seek urgent medical attention to improve your chances of a successful recovery.
Finding a Crohn’s Disease Specialist Near Me
When dealing with Crohn’s disease, find a gastroenterologist who truly understands the condition. They’ll help with an accurate diagnosis, manage any complications, and create a treatment specifically for you. With the latest therapies, they can help ease your symptoms and improve your quality of life.
How to Find Crohn’s Disease Specialist in Your Area
- Ask your friends, family, or colleagues.
- Ask your primary care physician or general practitioner for a referral.
- Contact your insurance provider for nearby gastroenterologists covered under your plan.
- Use sites like the Crohn’s & Colitis Foundation and WebMD to find specialists based on your location.
- Search online for “crohn’s disease specialist near me,” “crohn’s specialist near me,” or “crohn’s disease doctor near me.”
- Read reviews of local doctors online and schedule consultations to get to know more about them.
- Your Crohn’s disease specialist should be board-certified in Gastroenterology.
How Do You Get Crohn’s Disease?
While Crohn’s disease can strike anyone at any age, disease onset is most common between the ages of 15 and 35 in both men and women.
You may have a higher chance of developing Crohn’s disease if you:
- Smoke
- Have family members with an IBD
- Consume a high-fat diet
- Use NSAIDs regularly
- Have autoimmune disease
- Are white
- Live in a developed country, in an urban area, and in northern latitudes
- Have vitamin D deficiency
Additionally, long-term exposure to polluted air is believed to be associated with the incidence of Crohn’s disease. However, this issue should be clarified further in future studies.
How to Prevent Crohn’s Disease?
Early identification of individuals at high risk for disease development is critical for preventing symptoms of Chron’s disease and avoiding potentially severe and long-term complications. If you or your first-degree relative has previously experienced gastrointestinal problems, or if you are currently having digestive issues, we strongly recommend you schedule an in-person consultation with one of our expertly trained gastroenterologists to establish an early diagnosis and start appropriate treatment.
Managing Crohn’s Disease
Aside from early detection, there are certain self-care preventative measures you can try to slow the progression of early Crohn’s Disease and lengthen the time between flare-up episodes.
Nutritional Considerations:
- Ensure adequate intake of essential vitamins and minerals. Identify and address potential nutrient deficiencies through blood tests and dietary adjustments or supplementation.
- Consider elimination diets or food sensitivity testing under professional guidance to identify and avoid trigger foods that exacerbate symptoms.
- Focus on a balanced diet rich in fiber, prebiotics, and probiotics to support a healthy gut microbiome. Depending on the illness, diets like low FODMAP or other restricted diets may be needed.
Lifestyle Adjustments:
- Exercising regularly is also a good way to reduce or prevent disease activity and relieve associated psychological distress. Consider low-impact activities such as yoga, cycling, and swimming.
- Prioritize quality sleep and establish a consistent sleep schedule.
- Reduce or eliminate harmful habits such as smoking and excessive alcohol consumption.
- Learn to manage time effectively and prioritize tasks to reduce stress and improve productivity.
Psychological Support:
- Seek professional counseling or therapy to address emotional challenges, stress, anxiety, or depression. Connecting with support groups can help gain insights and find emotional support from others facing similar challenges.
- Practice stress-reduction techniques, such as meditation, yoga, deep breathing exercises, or mindfulness.
- Learn healthy coping mechanisms to manage difficult emotions and develop strategies to build resilience and maintain a positive outlook.
It is a good idea to maintain oneself healthy by not smoking, seeking therapy, eating a balanced diet, and exercising often. Also, remember to see your doctor if you suspect something is wrong.
As some of NYC’s best-in-class gastroenterologists, our doctors provide effective, highly personalized, comprehensive care for Crohn’s disease. For more information about our practice or to schedule a consultation with one of our New York Crohn’s specialists, please contact our offices in Downtown, Midtown, and the Upper East Side.